During a special session on COVID-19 this morning, the Cobb County Board of Commissioners heard from Dr. Janet Memark, the District Health Director for Cobb & Douglas Public Health and Dr. Danny Branstetter, an infectious disease physician with the WellStar Medical Group.
The purpose of the special session was to gather information in preparation for the declaration of a State of Emergency in Cobb County.
Memark reported on the current situation with COVID-19 in Cobb County. She said that the number of confirmed cases in Georgia rose from 800 yesterday to over 1,000 today, and that with 82 cases Cobb County has the second highest number among counties in the state.
She reported that because of the limited number of tests possible in the state, the county can’t depend on testing to address the pandemic.
“So now we have had over 5000 tests performed in the state of Georgia,” she said. “The commercial labs have done over 3800 tests, and 631 of them have been positive.”
“The Georgia Public Health laboratory has done over 1200 tests, and 169 of those were positive,” she said. “When you look nationwide, the test positivity rate is between nine and 11 percent. In Georgia, we’re looking between 13 and 16 percent that are positive.”
“It has to do a lot with we’re testing our highest risk individuals, our first responders and our healthcare workers,” she said, “and so we do expect a little bit more positivity … but because we don’t have widespread testing, you’re going to see higher numbers there.”
She said that hospitals don’t have the testing capabilities that they would like, and that the drive-through testing being conducted by Cobb & Douglas Public Health can only do 30 tests per day.
“Even if you had all the tests that you wanted, the results are taking an inordinate amount of time. So we are getting tests between three days and over seven days that we’re not even getting results,” she said. “So you understand, this is not helpful to our situation.”
“We cannot make decisions if you can’t get as a test result in less than … 12 hours essentially.”
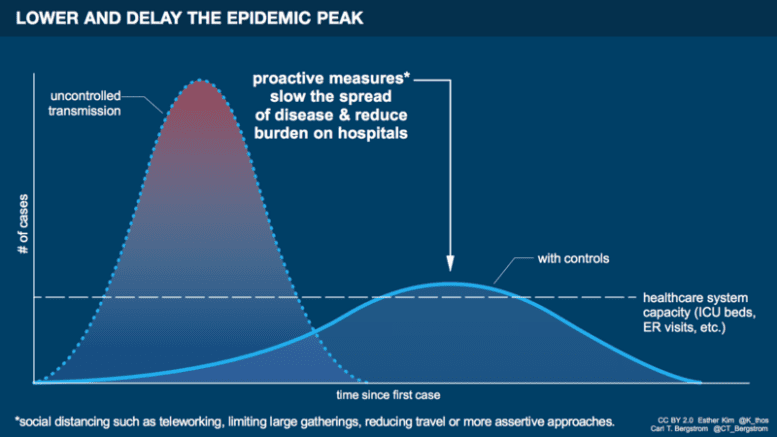
Memark then presented a version of the “flatten the curve” chart that demonstrates the goal in controlling a pandemic.
The difference between her chart and the one in this article is that Memark’s version was marked with a star showing the point in the timeline wjere Cobb is estimated to be in the pandemic.
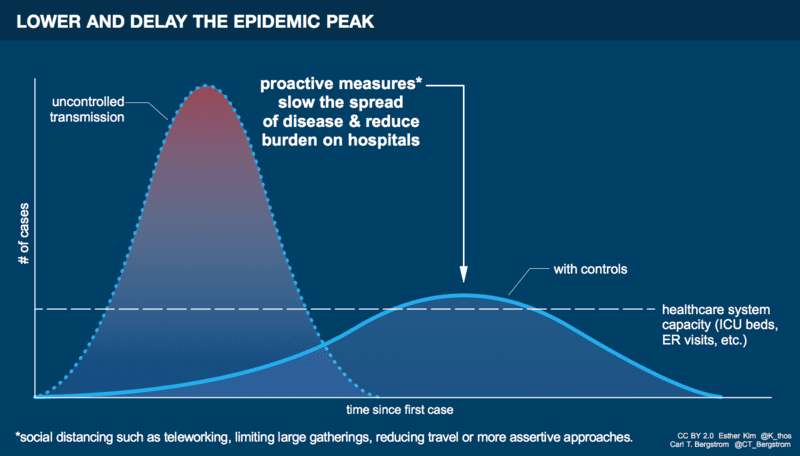
“And we tried our best estimate to put that little star there where we are,” she said. “So we are on the upswing of cases and we are just barely below our healthcare capacity at this time.”
“If we put in measures and try our best to put in as best measures as we can we can flatten that curve. The reason why flattening the curve is important is you keep it below that healthcare capacity.
“So we can at least care for as many people that need it as possible. Why does it matter? We have no vaccines, and we have no treatment. We have two hospitals in our county that are tertiary care centers, and they have less than 50 ventilators that are on hand to be able to take care of people.
“They have told us they can try to get some more but you’ve seen this situation in in New York, there might not be enough ventilators. We’ve over 760,000 people in our county alone. And this was a little bit of a surprise to me too.
“We have almost 6000 nursing home long term care facility and personal care home beds. That means we have 6000 people that are in vulnerable situations that are in in these homes. Why that’s important (is) t only takes a little bit and outbreak here or there to overwhelm our health system. Some of these places have over 200 beds apiece,” she said.
She said that even though little testing capacity exists, there is clear evidence of the spread of the disease.
“We … currently have three daycares that have positive cases. I have four nursing homes that have either positive or pending cases. And those are considered outbreaks. Each one in a nursing home is considered an outbreak,” she said. “I have multiple schools that have exposures. Thank God, they let the schools out. And so that has minimized that a little bit.”
“We have people in the hospital. Last I checked, we had over 60 people in one hospital that was under investigation or positive for COVID-19,” she said. “So without test, I’m telling you, we have community spread.”
She said that early in the pandemic, she could tell where each case came from. But now the spread is community-wide.
“So I’m asking you to act now. And I’m going to ask the doctor Branstetter to come and tell us what’s going on on his side and we can answer questions afterwards,” Memark said.
Dr. Branstetter began by saying that 80 percent of the people in the room would come down with COVID-19 at some point, and that the important thing is to slow the spread enough that the health systems don’t get overwhelmed.
“What we need to do is put in measures so our healthcare personnel can be available, the equipment, the supplies, the testing medications, the ventilators can be available to take care of each and every one of us,” he said. “The best measure for that to be instilled is social distancing. That’s the only way we’re going to be able to spread this out long enough. That way, when we begin, 80 percent of us … will all receive the highest care possible that we want as health care professionals to give to each and every one of us.”
“So why will 80 percent get it? Because we don’t have natural immunity. What’s 80 percent have to do with it?”
“80 percent is enough immunity within the community over time that it prevents it’s spread. (The) same concept goes for vaccinations. If we get high enough amounts of vaccination and protection within the community, then we’ll stop the spread.”
“It’ll buy us time, more time to develop a potential vaccine, more time to get better supplies and more supplies in, but also preserve the amount of capacity in each one of our facilities,” Branstetter said. “If we had another intervention that was simpler and less burdensome on our society, I’d be all for it. But right now this is the best thing we can do immediately as we try to weigh our expertise to care for those who will get infected.”